Anxiety Breakthrough: Pathogenic Gut Bacteria Linked to Anxiety, Depression, Panic Disorder & OCD—Evidence for a Novel, Effective Treatment
Trial registration: ClinicalTrials.gov ID: NCT07268729
Ethics board approval: Advarra – Protocol: Pro00084759
Abstract
Background
Anxiety, depression, panic disorder and OCD are among the most prevalent mental health conditions globally, affecting millions and imposing a substantial burden on individuals, families, and healthcare systems. These disorders often manifest through recurrent, severe episodes of anxiety and fear, frequently accompanied by physical symptoms such as palpitations, chest pain, and dizziness, which can lead to significant functional impairment and diminished quality of life. While current treatment options include pharmacotherapy and cognitive-behavioral therapy, response rates vary, and many patients experience residual symptoms or adverse effects, leading to high rates of treatment discontinuation. Furthermore, the growing recognition of treatment-resistant anxiety, depression, panic disorder and OCD highlights an urgent need for innovative, evidence-based therapies that provide sustained relief without compromising safety.
Introduction
Anxiety, depression, panic disorder and OCD are pervasive and debilitating chronic mental health conditions, affecting approximately 20% of the global population over a lifetime. Characterized by episodes of intense fear and physical symptoms such as heart palpitations, shortness of breath, and dizziness, these disorders can severely impact daily functioning, interpersonal relationships, and overall quality of life. Individuals with these conditions are also at increased risk for comorbidities including depression, substance use disorders, and cardiovascular disease, further complicating their clinical profile and necessitating more comprehensive treatment strategies. Despite the availability of pharmacotherapy, such as selective serotonin reuptake inhibitors (SSRIs) and benzodiazepines, alongside cognitive-behavioral therapy (CBT), there remain substantial challenges in achieving and maintaining symptom relief. Response rates vary widely, and a significant proportion of patients experience partial or inadequate relief, with some exhibiting treatment-resistant symptoms. Moreover, pharmacological treatments can be associated with side effects like weight gain, fatigue, and cognitive impairment, which may lead to discontinuation or non-adherence. These limitations highlight a critical need for alternative or adjunctive interventions that can provide more effective, sustainable, and safer outcomes. This trial was therefore designed to assess the prevalence of pathogenic gut bacteria among patients with anxiety, depression, panic disorder and OCD compared to healthy controls.
Objective
This study aims to investigate the etiology of anxiety, depression, panic disorder and OCD, providing new evidence and insights into the root causes and effective treatments, potentially offering a novel approach to achieving complete recovery.
Findings from this study are expected to advance clinical understanding and expand treatment options for anxiety, depression, panic disorder, and OCD, with the potential to move from symptom management toward symptom resolution.
Types of Depression
In this study, we investigated depressive symptoms occurring in the context of anxiety and panic disorder. These symptoms were distinguished from Major Depressive Disorder (MDD), a clinical diagnosis characterized by persistent sadness, loss of interest, and other debilitating symptoms such as sleep/appetite changes, low energy, and difficulty concentrating, lasting several weeks and affecting daily functioning.
Major Depressive Disorder (MDD) has been observed to arise via the gut–brain axis following intoxication from ingestion of non-food substances that cause severe irritation and disruption of the small intestine. Exposures observed to be associated with onset of depressive symptoms include: Bodybuilding supplements/hormones and protein powders; overuse of certain medications (aspirin); certain supplements and herbs; and prolonged alcohol misuse. Symptom resolution has been observed to occur with recovery of the small intestine following the acute irritative insult.
Rather than viewing the gut–brain axis as a minor influence, we observed findings consistent with a central role of intestinal processes in mood state regulation. Accordingly, we frame the small intestine as functionally integrated with brain processes and as is the principle mechanism to the biology underlying mood. We further hypothesize that intestine-based neuronal networks mirror key functional properties of brain-based networks and operate in parallel, contributing directly to mood regulation.
Design
Randomized controlled trial.
Methods
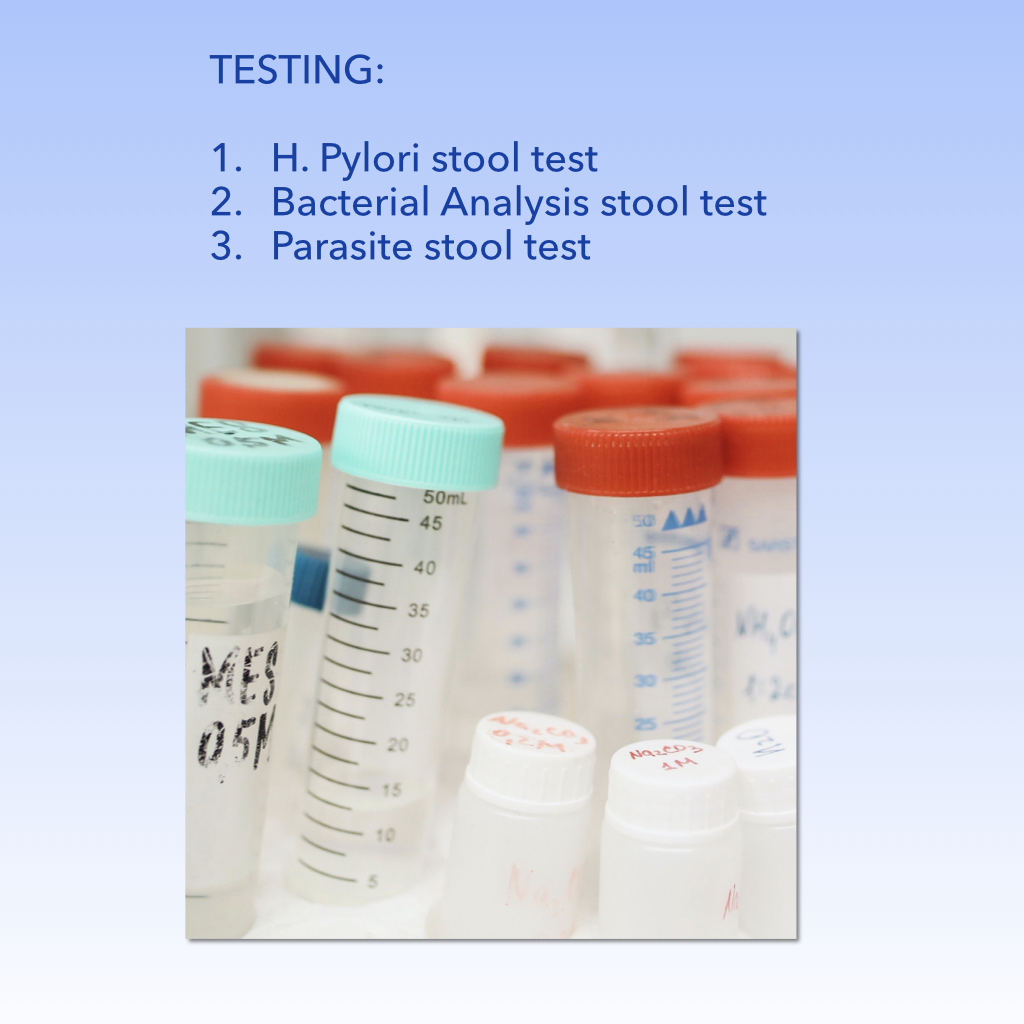
A total of 500 participants aged 18–65 were recruited and randomized. Groups included: (1) healthy controls with no psychiatric history, (2) patients with clinically confirmed anxiety, depression, panic disorder and OCD, and (3) patients under ongoing treatment. Stool analysis was performed to detect gut pathogens. Primary outcome: presence of pathogenic gut bacteria. Secondary outcomes: symptom reduction, and eradication.
Results
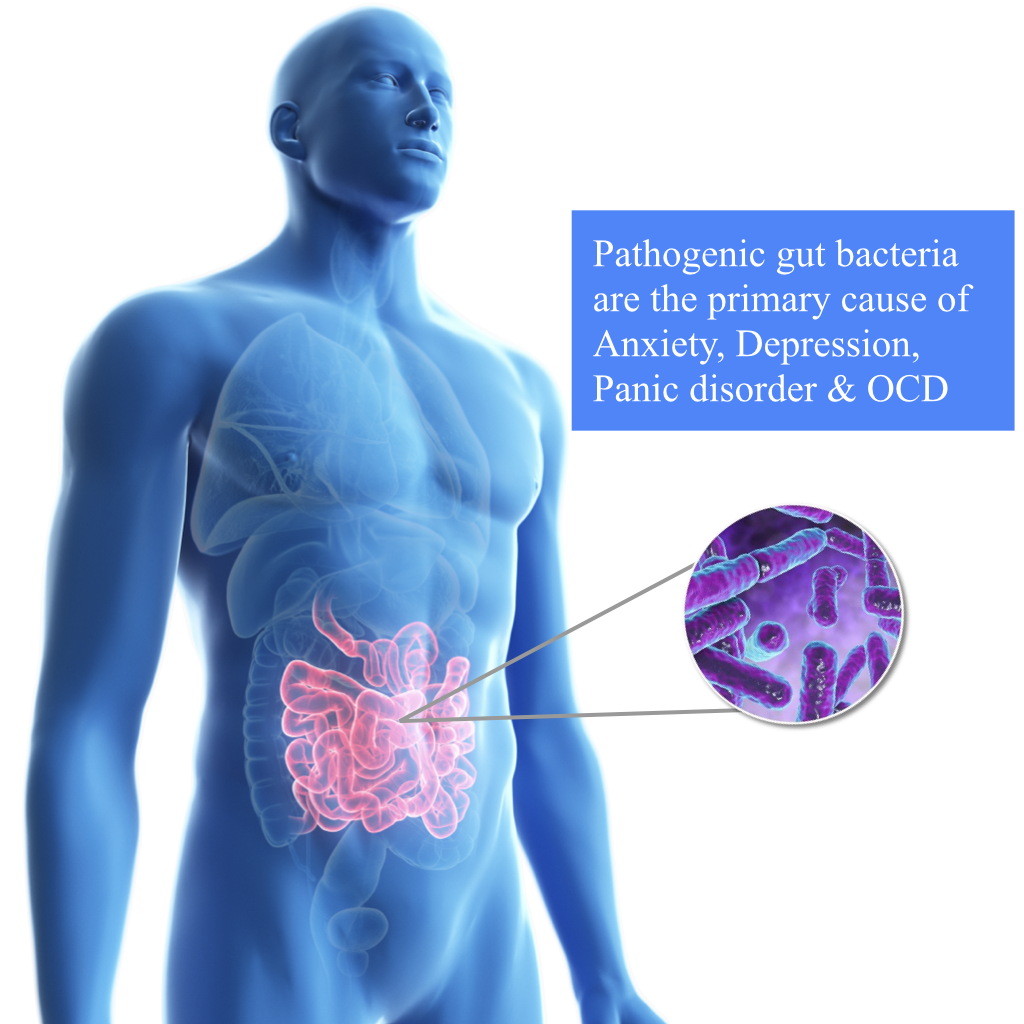
Healthy participants harboured no pathogenic bacteria in their guts. Among symptomatic groups, 95–97% carried pathogenic bacteria (73–78% Helicobacter pylori; 16–21% Alpha-Haemolytic Streptococcus). The majority of participants harboured multiple pathogens in their guts.
Discussion
The study’s findings provide strong evidence that pathogenic bacteria are directly linked to symptoms of anxiety, depression, panic disorder and OCD.
Intervention and Follow-up
Participants whose laboratory analyses confirmed pathogenic gut bacteria received treatment with targeted antibiotics.
Outcomes
Subsequently, participants were reassessed to determine changes in mental health status, specifically symptoms of anxiety, depression, panic disorder and OCD.
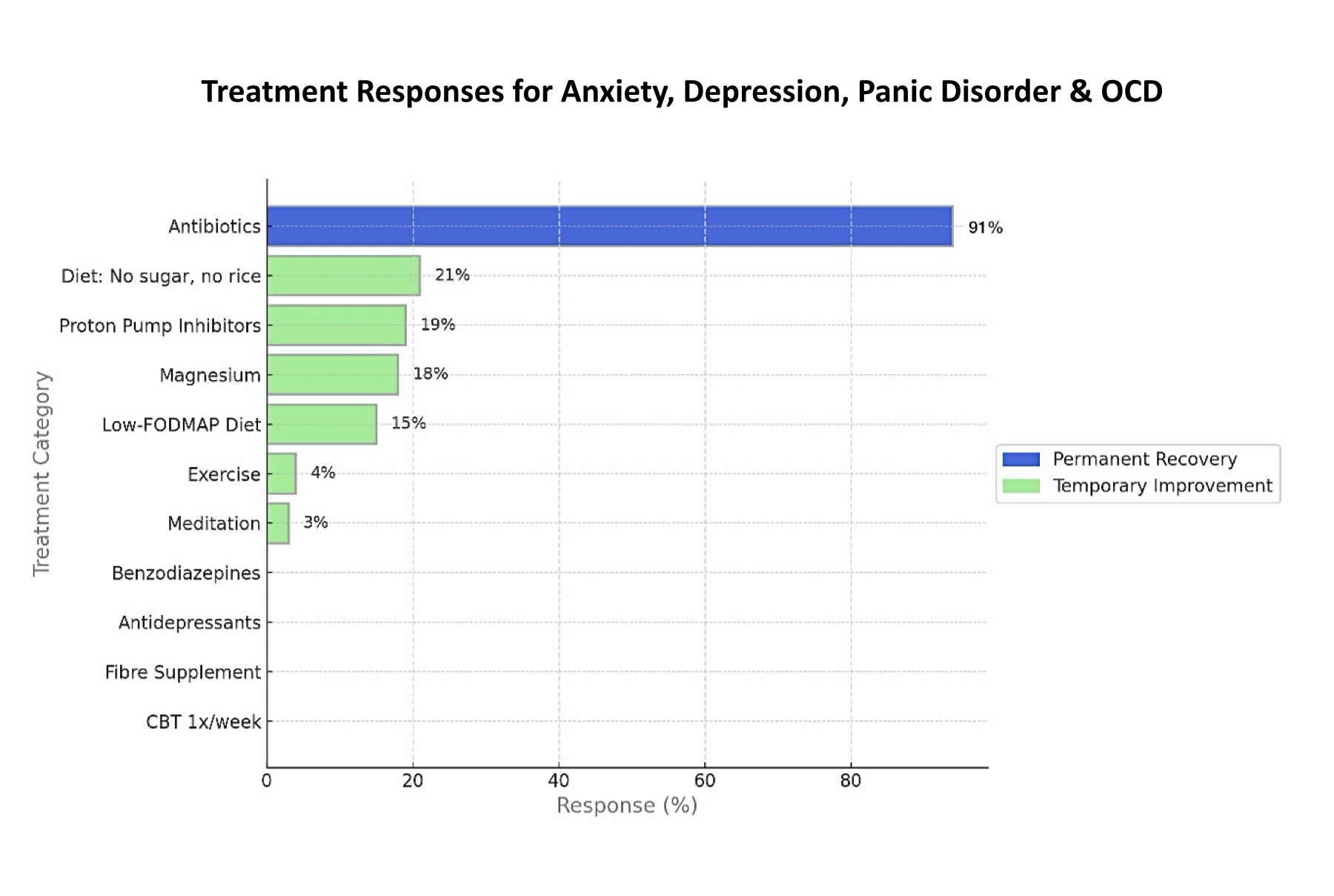
The following Figure presents the distribution of administered treatments and illustrates the relative improvements observed across the three symptom domains (anxiety, depression, panic disorder and OCD).
Results
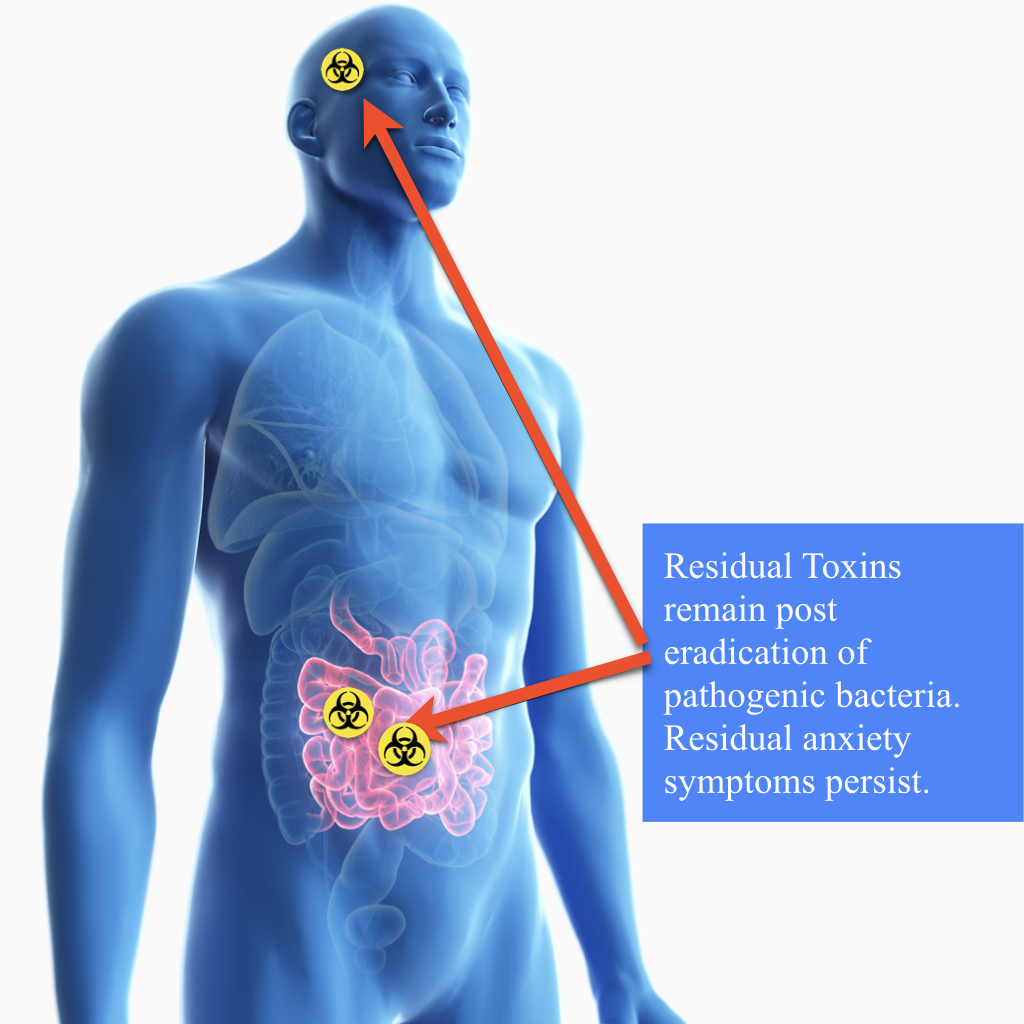
Antibiotic therapy achieved 91% sustained recovery, though some residual symptoms remained.
Helicobacter pylori (H. Pylori) infection was eradicated following standard triple therapy consisting of lansoprazole, clarithromycin, and amoxicillin administered according to guideline-based dosing. Alpha-hemolytic Streptococcus spp. was subsequently eradicated after targeted antibiotic therapy with clindamycin (300 mg) and cefuroxime axetil (500 mg). Treatment response was confirmed based on post-therapy clinical and/or laboratory assessment.
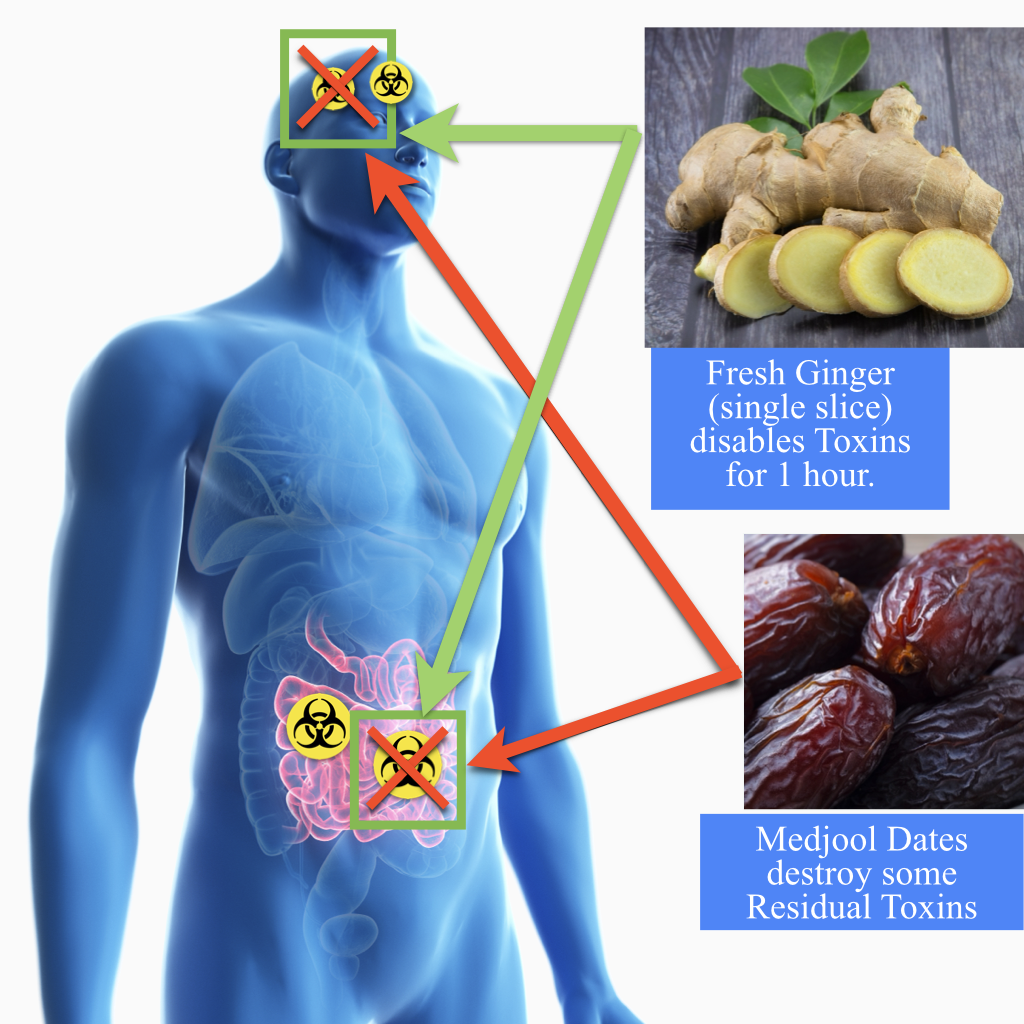
Following antimicrobial eradication, adjunctive supportive interventions were assessed. Fresh ginger was associated with an approximate 98% reduction in symptom severity, with effects described as transient and lasting about 1 hour. Consumption of Medjool dates was associated with an estimated 56% lasting reduction in symptom severity. Probiotic use was associated with an estimated 97% sustained reduction in symptom severity during follow-up. The combination of these interventions was associated with an approximate 98% sustained reduction in overall symptoms. No adverse events were reported.
At baseline, healthy participants who had no reported history of anxiety, depression, panic disorder, or obsessive–compulsive disorder. Following infection with pathogenic gut bacteria (including H. pylori and alpha-hemolytic Streptococcus spp.), anxiety symptoms began within 12 hours.
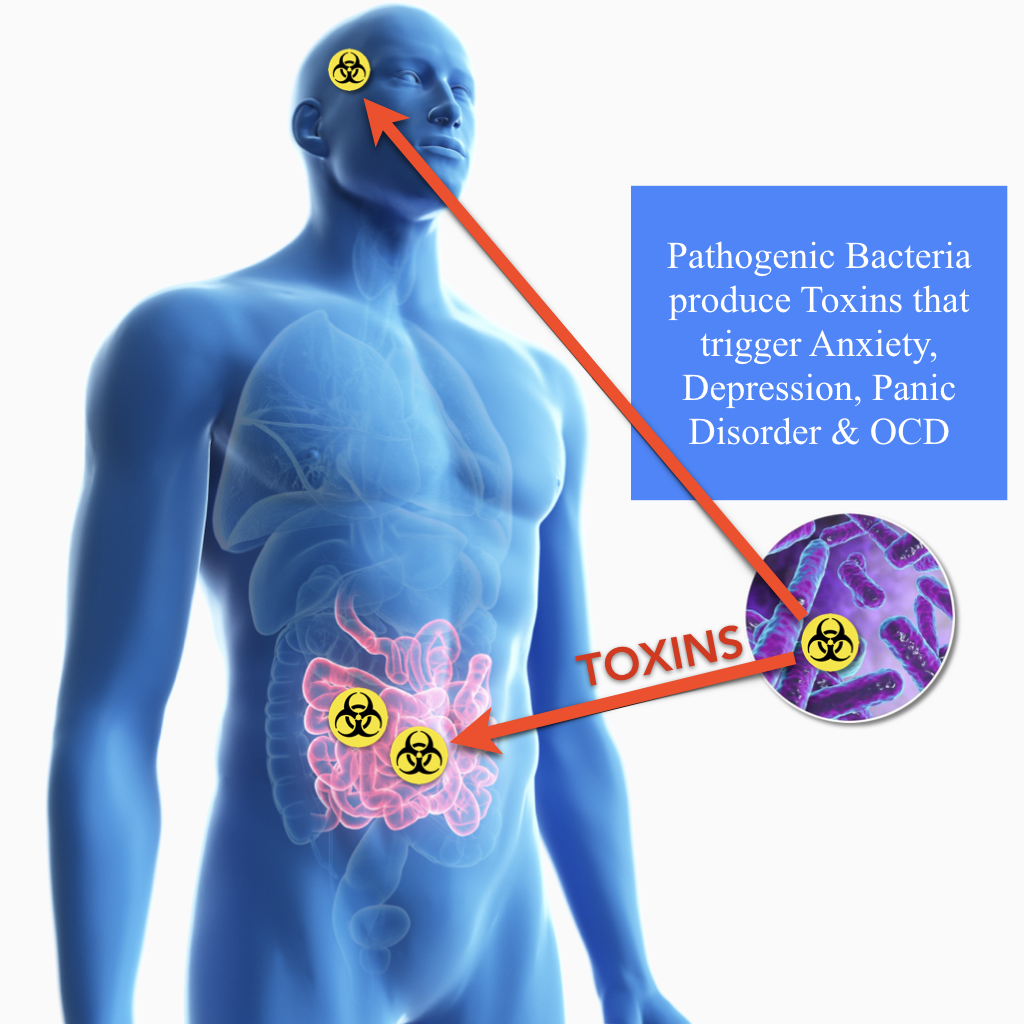
Pathogenic gut bacteria, including H. pylori, were found to produce bioactive molecular compounds with neurotoxic properties affecting the nervous system, manifesting as symptoms of anxiety, depression, panic disorder, and obsessive–compulsive disorder. Additionally, pathogenic gut bacteria were observed adhering to small-intestinal epithelial cells, with associated increases in nervous system tension and a higher occurrence of panic attacks. Conclusions
This trial provides strong evidence linking pathogenic bacteria in the gut to anxiety, depression, panic disorder and OCD. Eradication of gut pathogens with antibiotics, followed by detoxification with natural remedies, produced full recovery in nearly all patients. This approach represents a paradigm shift from symptom management toward curative treatment. Trial Registration: ClinicalTrials.gov ID: NCT07268729 Funding: Sponsored by MedBliss Research Network.
Methods
Trial Design
This study was conducted as a randomized controlled trial. Randomization was computer-generated, and allocation concealment was maintained using identical packaging.
Participants
The study included 500 participants aged 18–65, recruited across multiple clinical settings. Groups: (1) healthy controls, (2) clinically diagnosed patients, (3) patients under ongoing treatment.
Harms
No significant adverse events were reported.
Interventions
Stool test kits were provided for analysis.
Outcomes
Primary: presence of pathogenic gut bacteria. Secondary: symptom reduction, residual symptoms, response to detoxification remedies.
Sample Size
500 participants ensured statistical power for subgroup analysis.
Randomization and Blinding
Computer-generated randomization; participants and investigators blinded until analysis.
Statistical Methods
Chi-square tests and logistic regression models. Significance at p < 0.01.
Results
Participant Flow
500 participants were enrolled with balanced distribution.
Baseline Data
Healthy participants: no bacteria. Symptomatic: 95–97% with pathogens (73–78% H. pylori; 16–21% Alpha-Haemolytic Streptococcus; 76–79% multiple pathogens).
Numbers Analyzed
All 500 participants included.
Outcomes and Estimation
Antibiotics: 91% sustained recovery. Ginger: temporary complete recovery (98%). Dates: lasting relief (56%). Probiotics: permanent residual symptom eradication (97%). Combined: 98% complete recovery.
Discussion
Findings demonstrate a direct link between gut pathogens and anxiety, depression, panic disorder and OCD. Antibiotics were highly effective, and natural remedies eliminated residual symptoms. This supports the gut-brain axis as a mechanism in mental health and suggests a paradigm shift from symptom management to symptom resolution.
Figures:
Other Information
Ethics and Biosafety
Conducted in accordance with the Declaration of Helsinki. Written informed consent obtained. No biosafety risks.
Research in Context
Evidence before this study: Existing treatments provide incomplete relief. Gut microbiota imbalance suggested in recent studies. Added value: First trial linking pathogenic gut bacteria to anxiety, and mood disorders. Eradication and detoxification achieves 98% recovery. Implications: Shifts paradigm toward curative treatment.
Conflict of Interest
The author declares no conflicts of interest.
Author Contributions
Hassan Kattan led the research, developed the methodology, and wrote the manuscript.
Funding
Sponsored by MedBliss Research Network.
Word count: 1187 words.


